EMR vs. EHR: What's the Difference?
The rapid rise of digitization in the health care industry has spurred many providers to upgrade and modernize their tech systems. From cloud-based DICOM image viewers to artificial intelligence (AI)-driven diagnostic tools, health care providers like you are increasingly turning to new and advanced solutions to enhance their operations.
Two of those solutions are electronic medical records (EMR) and electronic health records (EHR). Although the terms are often used interchangeably and share many similarities, the two are actually different types of software tools.
This post will compare and contrast EHR vs EMR systems, so you can understand the most important differences between the two and how it can impact your practice.
What Is an Electronic Medical Record System (EMR)?
At their most straightforward, electronic medical record systems (EMR) are digital replacements for patients' paper charts.
An EMR typically contains clinical data about the patient, such as:
- Allergies
- Medications
- Diagnostic information
Most EMRs are specific to one facility or health care organization, with limited capabilities for interoperability between different members of a patient's care team. If a provider wants to add new information about a patient's recent surgery, for example, they will need to manually contact the surgeon's office and input that data into their system.
Some of the most important benefits of using an EMR include:
- Improved operational efficiency
- Enhanced coordination between facility staff
- Reduced risk of medical errors
- Increased treatment effectiveness
- Custom configurations for specialists
EMRs can also integrate with other solutions in your tech stack to provide a more centralized location for all your data. Facility staff can access all the most relevant patient data from one source rather than having to spend unnecessary time searching through various different applications.
What Is an Electronic Health Record System (EHR)?
An electronic health record system (EHR) is a more extensive solution that includes all the capabilities of an EMR and more. EHRs store a more comprehensive range of patient-level information, including but not limited to:
- Patient demographics
- Diagnoses
- Medications
- Vital signs
- Laboratory data
- Problem lists
According to one study from the Office of the National Coordinator for Health Information Technology (ONC), approximately 96% of U.S. hospitals have made the switch to EHRs from paper charting and legacy EMRs.
EHRs enable providers and organizations to share this data with other members in a patient's care team, including general care providers, specialists and more. All authorized users can edit and add to patient records to provide a more comprehensive view of a patient's entire health history.
Some of the biggest benefits of an EHR include:
- Patient involvement: EHRs enable patients to understand and take charge of their condition. Patients can access their data with more advanced EHRs, which can motivate them to continue following prescribed treatments and improve their outcomes.
- Data-driven decision-making: EHRs store more comprehensive patient data, which enables practitioners to make more informed decisions regarding diagnoses and treatments.
- Streamlined emergency care: Because EHRs contain more historical patient data than EMRs, emergency department teams can gain immediate access to critical information, such as severe allergies and other preexisting conditions that could impact care regardless of their geographical location.
EHRs can also integrate with other solutions in your tech stack, and in some cases they can even replace those solutions due to their more comprehensive capabilities.
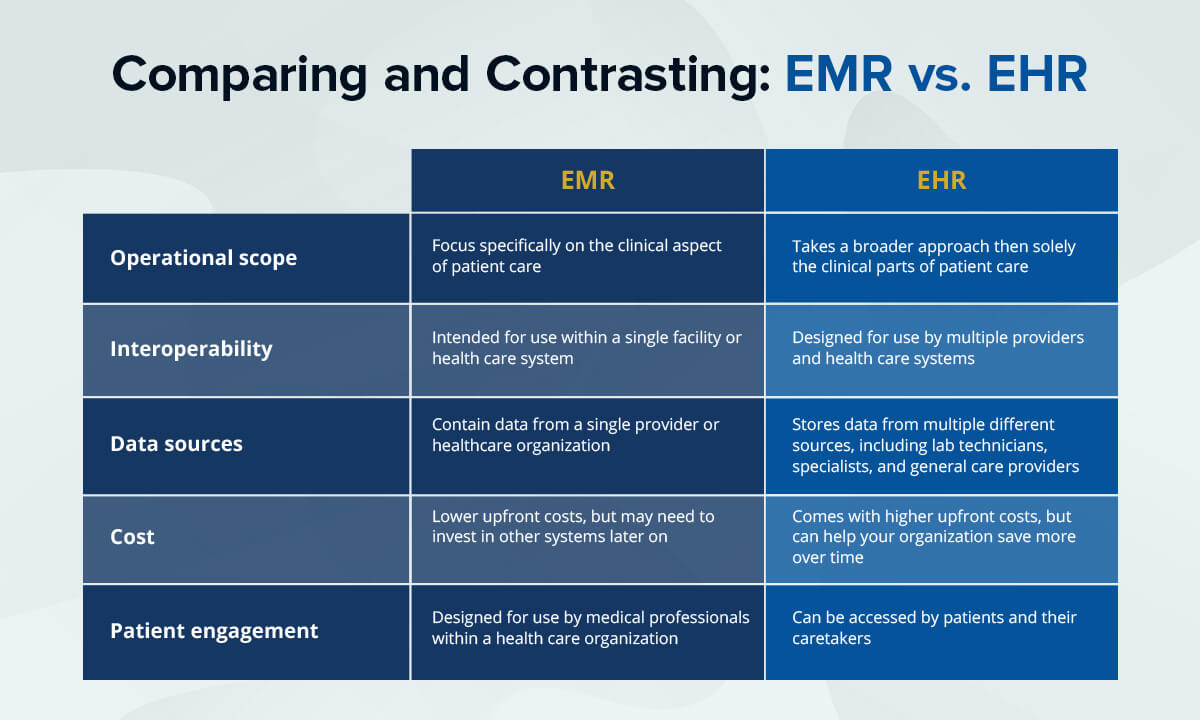
Comparing and Contrasting: EHR vs. EMR
Which system is best for your health care organization? A side-by-side comparison will help illustrate the key differences between an EHR and an EMR, so you can make the best decision.
EHR and EMR Differences
Some of the most significant differences between EMR and EHR include:
- Operational scope: EMRs focus specifically on the clinical aspect of patient care, meaning they store information related to past and current medications, diagnoses and underlying conditions. EHRs take a much broader approach.
- Interoperability: EHRs are designed for use by multiple providers and health care systems, which enables a patient's entire care team to collaborate in patient treatment. EMRs, on the other hand, are intended for use within a single facility or health care system.
- Data sources: While EMRs contain data from a single provider or healthcare organization, EHRs can store data from multiple different sources, including lab technicians, specialists, general care providers and more.
- Cost: Because EHRs have a broader operational scope, they typically come with higher upfront costs than EMRs. However, their increased interoperability and expanded capabilities can limit the need to invest in other similar systems, which can help your organization save more over time.
- Patient engagement: EMRs are designed specifically for use by medical professionals within a health care organization, while EHRs can be accessed by patients and their caretakers.
EHR and EMR Similarities
EMRs and EHRs also share many similarities, such as:
- Patient data storage: Although the scope is different for each system, both EMRs and EHRs enable providers to store and access patient data in a centralized location for simpler access and analysis.
- Remote access: Modern EMRs and EHRs are cloud-based, so providers can access them from multiple different devices and locations.
- Greater efficiency: Both EMRs and EHRs consolidate patient data into one single source of truth, which gives providers easier access to the information they need to make critical care decisions.
- Cost savings: Because EHRs and EMRs enable practitioners to record and store patient data digitally, they eliminate the need to continue purchasing and retaining paper files for operations like charting and compliance management.
- Data security: To protect patient information, both EMRs and EHRs must adhere to stringent data security and privacy regulations like HIPAA and PCI-DSS.
- Software integrations: A cloud-based EHR or EMR can integrate seamlessly with other systems in your tech stack, such as insurance, billing, image viewing and scheduling programs. This integration centralizes all your patient data into one single source of truth, creating a frictionless user experience.
Enhance Your Health Care Tech Stack With Candelis
Understanding the difference between EHR and EMR systems is essential for creating a health care tech stack that works for your organization and your patients. The next priority is choosing software solutions that integrate with that system.
The ImageGrid and ImageView product lines from Candelis are scalable, highly versatile data storage, DICOM routing and image viewing solutions that are designed to integrate seamlessly with your existing workflow. Both solutions integrate seamlessly with modern EMRs and EHRs to streamline your care processes and enhance your capabilities.
See how Candelis can help your practice enhance efficiency and improve patient care quality. Contact us today to book a free demo or talk to an expert about any of our products.

- Log in to post comments
